The Pathophysiological Mechanisms of Presbycusis
In a previous article, we discussed presbycusis, its impact on hearing and the lives of those affected, as well as approaches to prevention and treatment. In this article, we will examine presbycusis from a pathophysiological perspective. Pathophysiology is a branch of medicine that aims to explain how bodily functions are altered when a disease or condition occurs, whether it is physical, chemical, biological, neurological, or even psychological in nature. Let’s begin with a few definitions.
- Definitions
Pathophysiology
“Patho” comes from the ancient Greek word “pathos,” which translates to “disease” or “pain.”
“Physio” is a prefix derived from the ancient Greek word “phusis,” meaning “nature.”
“Logy” is derived from the ancient Greek word “logos,” meaning “study” or “discourse.”
Thus, pathophysiology is defined as the study of the nature of diseases.
Presbycusis
“Presby” is a prefix derived from the ancient Greek word “presbus,” meaning “aged” or “old.”
“Acusis” comes from the ancient Greek word “akoe,” meaning “hearing” or “the ability to hear.”
Thus, presbycusis is defined as a decline in hearing ability related to aging.
Although presbycusis is not categorized as a disease, as it occurs naturally with aging, certain pathophysiological mechanisms of normal aging can explain its origins. In this article, we will present the basic anatomical concepts related to hearing, which will then allow us to explain how presbycusis affects the structures of the ear. To do this, we will review the different types of presbycusis identified in the scientific literature and detail the specific implications of each type on the auditory health of those affected.
2. Basic Anatomical Concepts
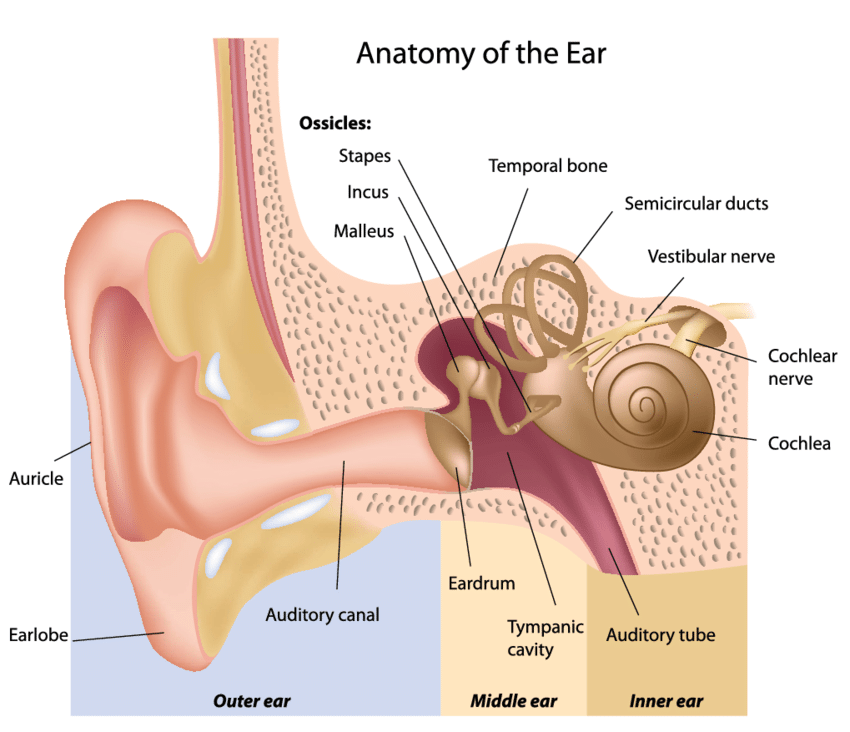
The outer ear consists of the auricle, which captures sound waves, and the auditory canal, which directs these waves towards the eardrum.
The middle ear is the intermediary between the external and inner ear. It includes the eardrum, the ossicles (malleus, incus, and stapes), and the auditory tube. Its primary role is to amplify sound vibrations by converting them into mechanical energy. The stapes, acting like a piston, reproduces the eardrum’s movements induced by sound vibrations, thus transmitting these vibrations to the fluids contained in the inner ear (the perilymph and endolymph).
The inner ear, nestled within the temporal bone, is a hollow bony structure often referred to as “the labyrinth.” It is divided into two parts:
- The cochlea, responsible for hearing, resembles a coiled spiral.
- The vestibular organ, responsible for balance, is identifiable by its three semicircular ducts.
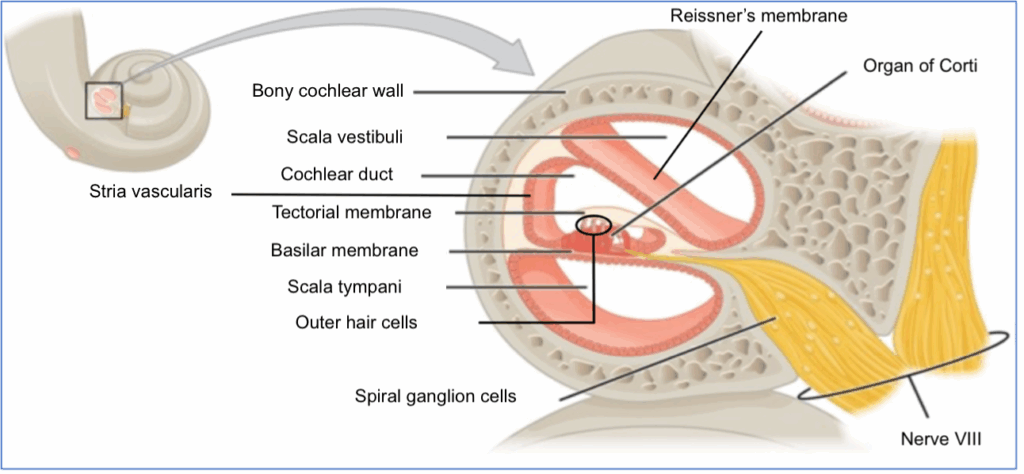
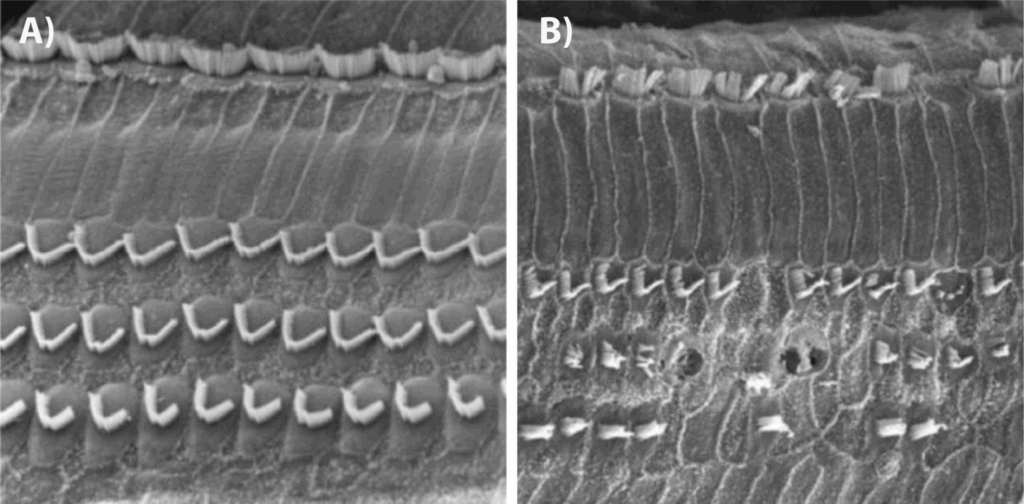
These two structures are contained within a membranous labyrinth, which mirrors the shape of the bony labyrinth. They communicate with the brain via small hair cells (Figure 2). These cells convert the fluid movements, either in the cochlea or in the vestibular system, into electrical signals that are then interpreted by the brain as sounds or motion.
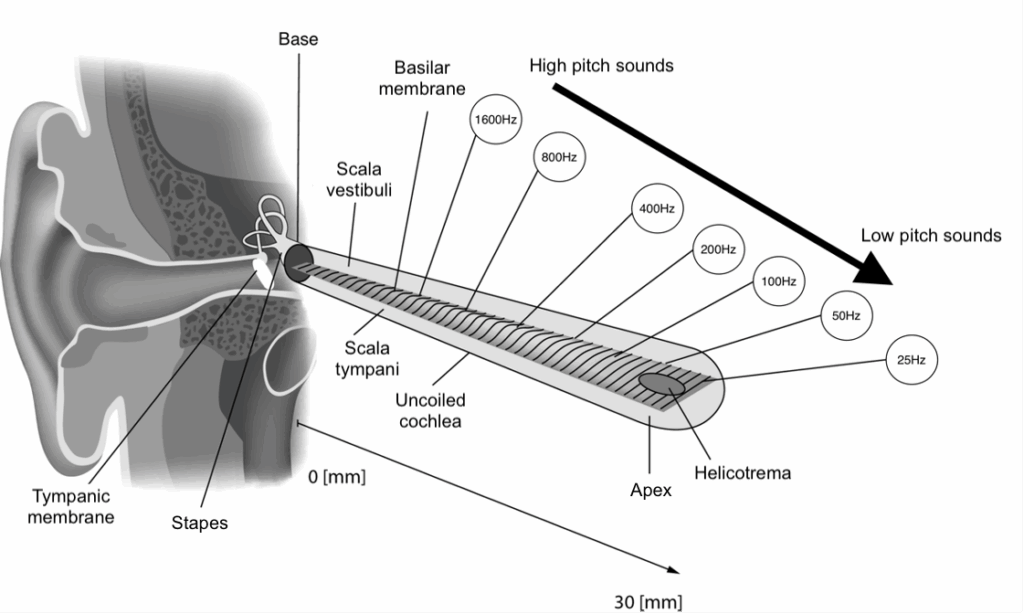
When a cross-section of the cochlea is made (Figure 4), it becomes apparent that it contains two ramps (the scala vestibuli and the scala tympani) and a duct (the cochlear duct) that are separated by very thin membranes, the Reissner’s membrane and the basilar membrane. Along the length of the cochlear duct, hair cells rest on the basilar membrane, which forms its floor. This canal is filled with a special fluid called endolymph. The scala vestibuli and scala tympani, located respectively above and below the cochlear duct, contain a fluid called perilymph. When sound vibrations enter the cochlea through the action of the stapes, they first propagate through this perilymph in the scala vestibuli. They then propagate into the endolymph of the cochlear duct, as the thin membranes allow the transmission of movement caused by the sound vibration. It is at this moment that the hair cells are stimulated. The vibrations then dissipate in the scala tympani, which, like the scala vestibuli, is also filled with perilymph. The formation of the endolymph in the cochlear duct is ensured by the stria vascularis, a highly vascularized tissue lining the lateral wall of the cochlear duct. The stria vascularis maintains the chemical balance of the endolymph, allowing the hair cells to function properly. In response to the movements of the basilar membrane induced by sound waves, these hair cells transmit nerve impulses to the spiral ganglion cells. These, in turn, direct the auditory information to the cochleovestibular nerve (also known as nerve VIII), which will carry the information to the brain.
3. Tonotopy: A Unique Physiological Mechanism
The cochlea is a remarkable organ, particularly distinguished by its tonotopic organization, meaning that the location of the hair cells on the basilar membrane determines the sounds they are responsible for processing. High-pitched sounds stimulate the hair cells at the entrance (base) of the cochlea, while low-pitched sounds affect those located at its end (apex) (see Figure 5). When a high-pitched sound creates a “wave” in the inner ear fluids — the perilymph and endolymph — this wave reaches its peak quickly, activating the cells at the base of the cochlea, resulting in the perception of a high-pitched sound. Conversely, a low-pitched sound wave reaches its peak deeper within the cochlea, stimulating the cells in the region of the apex, leading to the perception of a low-pitched sound. Thanks to this tonotopic organization, our ear can discern a wide range of frequencies, from 20 to 20,000 Hertz, making our sense of hearing highly precise.
Tonotopy
“Tono” is a prefix derived from the Greek word “tonos,” meaning “tension” or “tone.” In this context, it refers to sounds.
“Topy” comes from the Greek word “topos,” meaning “place” or “location.” Here, it refers to the location of hair cells on the basilar membrane of the cochlea.
The term “tonotopy” therefore combines the notions of “sound” and “location” and refers to the organization of sounds on the basilar membrane of the cochlea.
4. Presbycusis: A Sensorineural Hearing Loss
Presbycusis is distinct from conductive hearing loss, which is due to dysfunction of the middle or outer ear. It is considered a sensorineural hearing loss because it affects the cochlea, the sensory organ dedicated to auditory perception, or the nerve fibers (spiral ganglia) that connect the hair cells of the cochlea to the auditory nerve. For a long time, presbycusis was viewed as the result of physiological changes in the ear related to aging. However, scientific advances have shown that, in addition to aging, it is caused by various factors, including genetic, pharmacological, and environmental factors, such as exposure to noise and toxic substances. Recent studies also suggest the involvement of the central nervous system. For instance, a decrease in auditory stimulation caused by presbycusis could lead to hyperactivity in the nervous system, causing tinnitus (ringing in the ears) or problems with sound tolerance (increased sensitivity to loud sounds). Magnetic resonance imaging (MRI) studies have demonstrated that prolonged sensory deprivation caused by presbycusis could lead to atrophy of the brain’s auditory regions, resulting in a process of cortical reorganization known as “brain plasticity.” Reduced connectivity between the two hemispheres due to brain aging could also cause difficulties in processing auditory information from both ears, complicating speech comprehension in noisy environments or the localization of sound sources. These disorders, such as tinnitus, difficulties in speech comprehension, or sound localization, are therefore closely linked to presbycusis. The brain mechanisms involved in presbycusis remain poorly understood but are the subject of extensive research.
5. The Different Types of Presbycusis
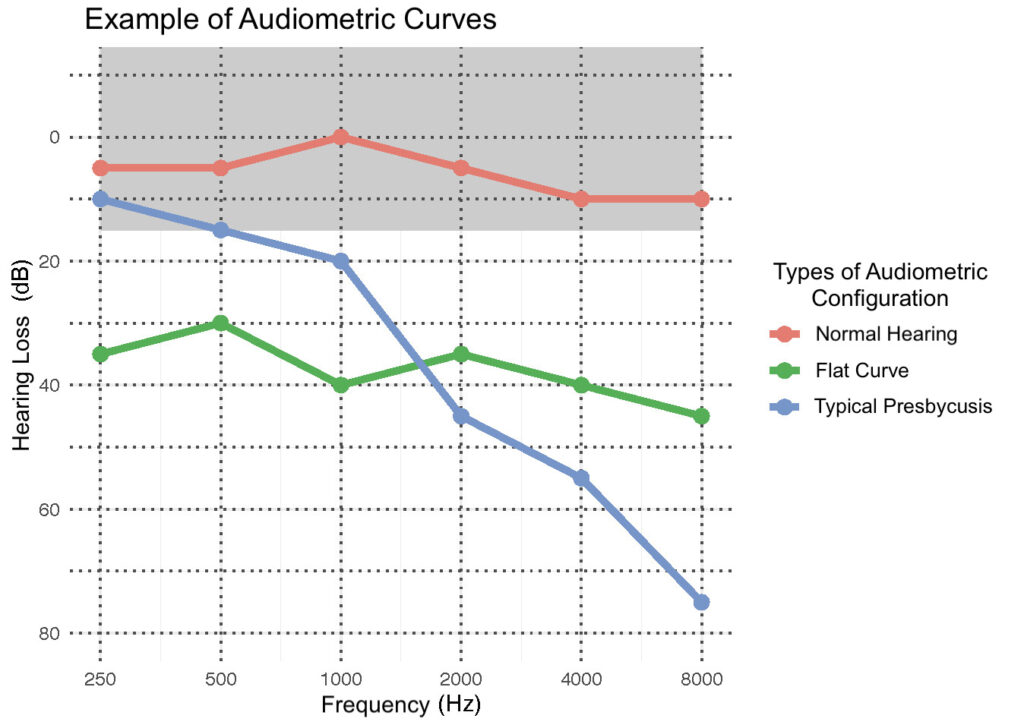
The different types of presbycusis presented in this section are based on studies conducted using cell samples taken from deceased individuals for whom audiograms were available (Figure 5). By comparing the cellular samples with the audiometric curves of these individuals, research teams were able to determine the impact of various cochlear impairments on auditory acuity as measured by audiometric evaluation.
Sensory Presbycusis
This form of presbycusis is characterized by the loss of outer hair cells at the base of the cochlea (approximately 0 to 12 millimeters). In more advanced stages, atrophy of the supporting cells of the organ of Corti can be observed. This loss results in a deficit in the perception of high-pitched sounds, but it rarely affects auditory acuity to the point of causing serious speech perception difficulties that are hard to compensate for with hearing aids (Figure 5, blue curve). This type of presbycusis is thought to be partly hereditary in both men and women. Cumulative noise exposure over a lifetime is the most significant contributing factor to this type of presbycusis, which is also considered the most common.
Neural Presbycusis (sometimes referred to as Central Presbycusis)
This type of presbycusis is defined by the loss of ganglion cells in the spiral ganglia (Figure 4). The loss of these cells can result in varying degrees of hearing loss depending on the location of the affected cells. Ganglion cell loss can occur along the entire length of the cochlea. This type of presbycusis is primarily manifested by speech perception difficulties that are more significant than the individual’s audiometric curve would suggest. Indeed, 75% of spiral ganglia can be affected without impacting auditory acuity as measured by pure-tone audiometry. The effects of this type of presbycusis generally become apparent in advanced age when the number of ganglion cells falls below a critical threshold. This presbycusis is more challenging to compensate for with hearing aids, especially when ganglion cell loss is more significant in the cochlear regions crucial for speech perception.
Metabolic Presbycusis (sometimes referred to as Strial Presbycusis)
This type of presbycusis is characterized by insufficient blood supply to the stria vascularis, leading to a chemical imbalance in the endolymph, which is necessary for proper hair cell function. Metabolic presbycusis is associated with a reduction in low-frequency hearing acuity because it affects the stria vascularis along the entire length of the cochlea (Figure 5, green curve). This type of presbycusis is most strongly associated with aging. It has a stronger hereditary component than sensory presbycusis and is more prevalent in women. Cardiovascular diseases are a significant contributing factor, particularly in women.
Mechanical Presbycusis
Mechanical presbycusis is thought to be associated with the stiffening of the basilar membrane and consequently the organ of Corti. This type of presbycusis is associated with when people presenting with a typical audiometric curve showing high-frequency loss, and no signs associated with other types of presbycusis. Some authors suggest that this pathophysiological mechanism is theoretical since there is very little evidence and scientific explanation for the phenomenon of basilar membrane stiffening. Additionally, the literature remains unclear about the precise manifestations of this type of presbycusis on the auditory acuity of those affected.
Mixed Presbycusis
Mixed presbycusis occurs when at least two of the characteristic traits of the aforementioned types of presbycusis are present (loss of hair cells at the base of the cochlea — loss of ganglion cells — dysfunction of the stria vascularis — stiffening of the basilar membrane). This form of presbycusis can therefore result in a wide variety of configurations, hearing losses, and specific difficulties associated with them.
Intermediate Presbycusis
This type of presbycusis involves submicroscopic alterations in intracellular organelles, dysfunctional cellular metabolism, a decrease in the number of synapses on hair cells, and chemical alterations in the endolymph. The audiometric curve associated with this type of presbycusis is relatively flat across all frequencies, with a slightly more pronounced drop in high frequencies. It could correspond to the green curve in Figure 5.
6. Conclusion
Presbycusis, although closely related to aging, is a complex auditory system impairment that encompasses various pathophysiological mechanisms. Its multifactorial nature, combining genetic, environmental, and metabolic elements, makes it challenging to understand and underscores the need to support research efforts to better grasp its nature. To date, only audiological evaluations, including pure-tone hearing acuity assessments, speech perception evaluations, and certain electrophysiological tests involving the use of electrodes, can provide clues about the type of presbycusis. Based on these evaluations, audiologists can guide their management and propose strategies tailored to each patient. While current technological advances do not yet allow us to determine the type of presbycusis in living individuals with great precision, they do offer a perspective on its manifestations and impacts on the daily lives of those affected.
Although we cannot yet fully prevent presbycusis, a better understanding of its mechanisms allows us to approach it with greater wisdom and optimism. It is essential to continue raising awareness about the importance of good auditory health throughout life, as presbycusis, while inherent to the aging process, can be influenced by modifiable factors such as noise exposure, risky pharmaceuticals, and toxic substances in our environment. In summary, knowledge, prevention, and education are our best tools to face the auditory reality of aging.
Suggested readings :
- Presbycusis
- Audiology and the work of audiologists
- The auditory cortex
- The central subcortical auditory system
- The peripheral auditory system
- Speech perception: a complex ability
- Difference between speech, language and communication
- The McGurk effect
- Being Deaf or hard of hearing
- The profession of speech-language pathologist
- Tour of our soundproof room
- Speech analysis
- Speech Perception in Noise: Facilitatory Mechanisms of the Peripheral Auditory System
- The cocktail party explained
- CIHR grant
- NeuroSPiN Project—Start of Data Collection