Who is the healthcare professional to consult for hearing loss, tinnitus, dizziness, and balance issues? The audiologist!
Audiology is a branch of rehabilitation sciences that focuses on hearing disorders, such as hearing loss, tinnitus, sound tolerance disorders, auditory processing disorders, communication disorders, and problems of vestibular origin, including dizziness and balance issues. If you suffered from ear infections in your childhood, chances are you have already consulted an audiologist, whether on the recommendation of your family doctor or at your parents’ initiative. As new parents, it’s likely that your infant was assessed as part of the Quebec program for newborn hearing screening (PQDSN), which aims to detect hearing problems present at birth. Moreover, if one of your loved ones, whether young or older, uses hearing aids, it was an audiologist who assessed their hearing and prescribed their hearing devices. Various concerns can lead a person to consult in audiology during their lifetime. In this article, we will define audiology by describing a typical audiological assessment and presenting the main areas of practice of the audiologist.
The Legal Framework of the Profession
In Quebec, audiologists is a regulated profession under the Professional Code. The Professional College responsible for access to the profession, regulation, and supervision of audiological practice is the College (“Ordre” in French) of Speech-Language Pathologists and Audiologists of Quebec (Ordre des Orthophonistes et Audiologistes du Québec : OOAQ). The mission of the College is to ensure the public’s protection concerning its members’ field of practice, notably by monitoring practice and supporting the maintenance of competencies. To legally hold the title and practice as an audiologist and carry out the activities reserved for this profession, it is imperative to hold a practice license issued by the OOAQ. This license attests that the audiologist meets the basic requirements to practise the profession. This permit also indicates that its holder is subject to a code of ethics, which is a set of ethical rules and principles of professional conduct. In Quebec, the Université de Montreal and Université Laval are the only universities that offer a master’s degree programs in audiology that qualify for the College practice license. These programs are specifically designed to prepare student individuals to become competent and qualified audiologists.
The Steps of the Audiological Evaluation
The audiological evaluation begins with an interview during which the audiologist asks the person not only about their auditory complaint but also about its impacts on their daily activities, social interactions, and overall quality of life. This information allows the audiologist to understand the needs and lifestyle habits that can positively or negatively influence the person’s hearing health and quality of communication. In short, this interview guides the audiologist in the choice of evaluations to be performed and recommendations to be formulated at the end of the consultation.
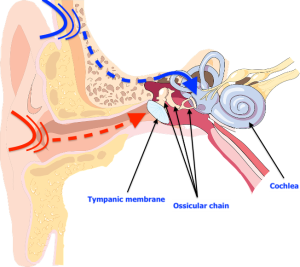
Before proceeding with the auditory evaluation, the audiologist performs a visualization of the external auditory canals (Figure 1). This step aims to ensure that the person’s auditory canals are clear and that there is no debris or cerumen plug obstructing the passage. Audiologists can indeed perform the extraction of a cerumen plug when it is likely to compromise the evaluation procedures. However, if you suspect that your ear is blocked by a cerumen plug, it is preferable to contact your audiologist to ensure they offer this service. Indeed, not all audiology clinics have the specialized equipment for cerumen extraction.
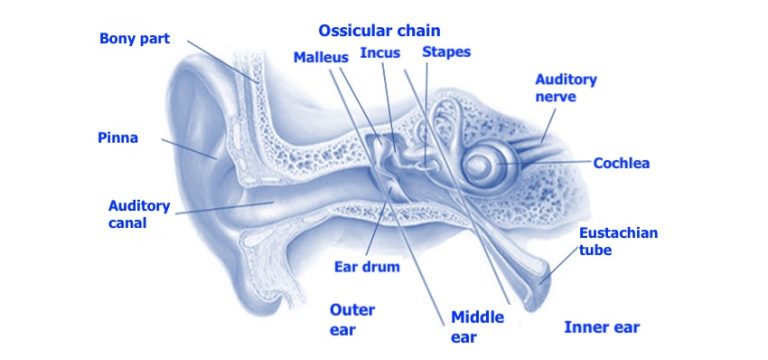
The next step is to assess the middle ear (Figure 1). Using the tympanometer (Figure 2), the audiologist can determine if the eardrum is mobile, if the middle ear pressure is balanced, and if the volume of the auditory canal is of normal size. For example, an immobile eardrum could suggest the presence of fluid in the middle ear, which is valuable information for the treating physician if they suspect middle ear infection in the person they referred for audiology. Negative pressure in the middle ear may indicate a dysfunction of the Eustachian tube (Figure 1) which no longer manages to properly balance the pressure. Negative pressure can result from a period of congestion during which the person would sniffle instead of blowing their nose. Finally, an abnormally high auditory canal size could indicate a perforation of the eardrum, as the space of the middle ear would be measured in addition to the space of the auditory canal. The results obtained during tympanometry are therefore crucial for the audiologist concerning the referrals they might make to other health professionals.
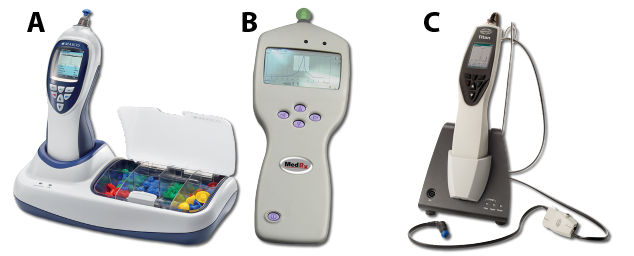
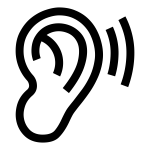
The evaluation of acoustic reflexes is generally carried out using the same device (Figure 2). This step aims to verify the presence of the ear’s protective reflex. By emitting sounds at a relatively high (but safe) volume in the person’s ear, the audiologist can observe the contraction of the stapedius muscle (Figure 3) through the movement of the eardrum. This small muscle comes into action when the cochlea detects a loud sound. Its mechanism consists of pulling on the ossicular chain composed of the stapes, incus, and malleus to immobilize it and thus reduce the vibrations transmitted to the cochlea. Given that the ossicular chain is attached to the eardrum by the handle of the malleus, this movement can be detected by the device. A failure of the acoustic reflex can sometimes indicate a problem with the ossicular chain, result from hearing loss, or in rarer situations, indicate a neurological disorder. In short, normal results in tympanometry and acoustic reflexes tell the audiologist that the middle ear’s mechanics are healthy.

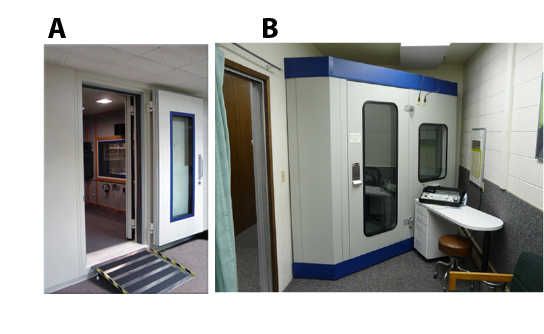
In a soundproof booth (Figure 4), the audiologist places a headset or earphones in the person’s ears. At this point, the patient is instructed to repeat the words presented by the audiologist or through pre-recorded material. The aim of this step is to determine the minimal volume at which the person can identify the words presented to them. This measurement will then serve as a reference to assess the validity of the results obtained in tonal audiometry.

Pure tone audiometry is undoubtedly the emblematic test of the audiological evaluation. It is carried out using an audiometer (Figure 5), which is a device primarily used to present pure tones (i.e., beeps) of different pitches at different volumes to determine the person’s minimal hearing threshold. The audiologist therefore asks the person to respond, by pressing a button or verbally, as soon as a sound is perceived, even if it is very faint. This test measures hearing acuity, i.e., the smallest volume (in decibels) at which a person can hear low and high pitch sounds relevant to speech perception (250 to 8000 Hertz). In certain situations, for example when a person experiences tinnitus in the absence of hearing loss, the audiologist may find it relevant to evaluate hearing acuity in the very high frequencies (9000 to 16,000 Hertz), given that tinnitus is a very common symptom associated with deafness.


While traditional pure tone audiometry measures hearing acuity by transmitting acoustic vibrations through the air to the eardrum via a headset, bone conduction pure tone audiometry directly stimulates the cochlea using vibration transmitted through the skull bones (Figure 6). A small vibrator, acting in the same way as a headset, is placed behind the ear on the mastoid process of the temporal bone. This test allows for a more direct measurement of the cochlea’s hearing acuity. If the audiologist observes a significant difference (at least 15 dB) between the hearing thresholds measured by air conduction and bone conduction, they will refer the person to an otolaryngologist for a more in-depth investigation of the cause of this discrepancy. A hearing loss caused by such a discrepancy is called “conductive hearing loss.” It can be caused, for example, by serous otitis media, where the middle ear is filled with fluid that interferes with the movement of the eardrum and ossicles. On the other hand, a hearing loss observed without a significant difference between measures by bone conduction and air conduction is called “sensorineural hearing loss,” as it involves the sensory organ of hearing: the cochlea. Sensorineural hearing loss can occur following prolonged exposure to high-amplitude noises, such as those found on construction sites or at rock music concerts. Sensorineural hearing loss can also occur naturally with normal aging. It should be noted that conductive hearing losses are sometimes medically treatable, while sensorineural hearing losses are permanent.

The evaluation generally concludes with auditory verbal tests, where the individual is asked to repeat words or sentences. These tests aim to simulate real listening situations or simply measure the recognition of similar words distinguished by a single sound. By adding white noise or pre-recorded babbling sounds, an individual’s auditory capabilities can be assessed in an acoustic context like a restaurant environment or in the presence of multiple speakers, for example. These measures can also be used to validate the effectiveness of hearing aids by comparing performance without hearing aids to that achieved with them.

After conducting the relevant tests related to the individual’s complaint, the audiologist verbally communicates the results. This stage involves explaining the results obtained from the various tests conducted and demonstrating to the individual how their results explain (or not) their complaint, while considering their auditory health history. The audiologist then shares their recommendations, which may include referrals to other health professionals, the prescription of hearing aids or assistive listening devices (such as amplified telephones, sound transmission systems for TV listening, portable microphones, etc.), as well as advice on good lifestyle habits related to hearing and communication. Subsequently, the audiologist prepares a report that includes the information collected during the interview, the results of the different tests, an interpretation of these results, an audiological conclusion (a professional opinion), a description of the interventions carried out, an intervention plan, and recommendations. This report can be sent to the individual and to other health professionals with their written consent.
Several other tests can be performed by the audiologist. The steps described above are part of a general assessment, such as what one might receive during a first visit in audiology. Additional tests include the test of otoacoustic emissions (which measures the activity of the hair cells in the cochlea), which can be performed in individuals suffering from tinnitus or in the context of newborn hearing screening. Indeed, the activity of these cells is usually predictive of healthy hearing. Electrophysiological measurements, called auditory brainstem response (ABR), can also be performed with electrodes if a problem at the level of the auditory nerve is suspected. This test can also be performed if the audiologist wishes to measure the hearing of a person unable to respond verbally or with a push-button, such as an infant or a severely disabled person. Finally, if a person’s complaint is related to dizziness or balance problems, a series of tests can be performed by audiologists working in clinics who have the necessary equipment for vestibular assessment.

Audiology services in private clinics are generally the most accessible in terms of waiting time. Whereas an audiology appointment in a hospital without a referral or emergency may require more than a year’s wait, an appointment in a private clinic can be obtained within 1 to 2 months. However, it is important to note that evaluation fees in private clinics are not covered by the Quebec Health Insurance Board (RAMQ) and can amount to approximately $100. Whether for a simple control evaluation, much like a visit to an optometrist, or for a more urgent situation, audiologists in the private sector are available to meet people’s needs in an efficient and prompt manner. Private clinics typically offer a wide range of services, from basic hearing assessments to hearing aid adjustments to rehabilitation programs. Individuals can benefit from personalized follow-up and can receive referrals to various health specialists according to their needs.

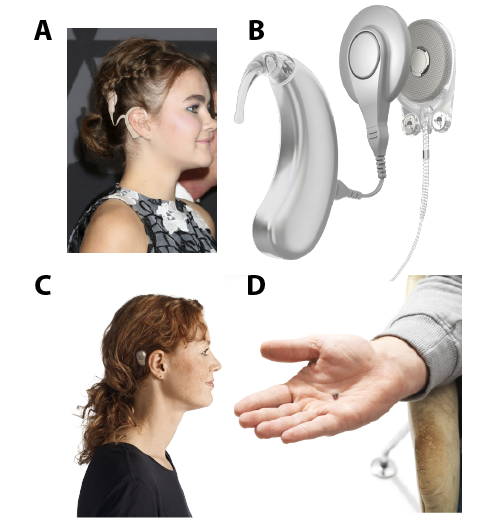
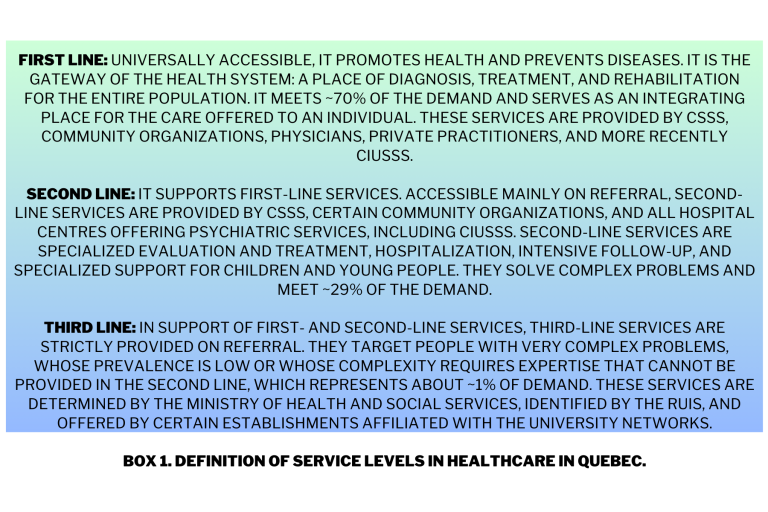
Hospitals are undoubtedly the places where the role of the audiologist is the most diversified and specialized. Here you will find pediatric audiologists who work notably in the Quebec program for newborn hearing screening to ensure appropriate follow-up of infants diagnosed with hearing loss. There are also audiologists responsible for monitoring and managing hearing problems associated with ototoxic treatments, such as chemotherapy. It is also in hospitals that you will find audiologists specializing in cochlear implants (Figure 7AB) and bone-anchored implants (Figure 8CD). These individuals are trained to assess candidates for these surgical procedures and ensure their pre-and post-operative follow-up. Audiology services in hospitals are generally obtained through referrals from health specialists such as family doctors or ENT doctors. Referrals can also come from front-line audiologists (Box 1) who wish to refer people to the cochlear or bone implant program, for example. It should be noted that audiology departments in hospital centres usually have front-line service like those offered in private clinics. In this sense, audiology services in hospital centres are both first- and second-line services.

Sometimes people, whether young or older, require longer-term audiological services. Indeed, consider a young child with deafness who needs to learn to use their prostheses and to communicate and socialize. One can also think of an adult diagnosed with deafness who needs to develop new communication strategies, adapt to wearing hearing aids, to the use of assistive listening devices, and to adapt their work environment to maintain their professional life. Rehabilitation services are available for anyone experiencing functional difficulties in terms of hearing and wishing to improve their condition. Generally, the referral to a rehabilitation centre is made by the first-line audiologist who documented the individual’s specific needs. Rehabilitation centres generally have multidisciplinary teams including audiologists, speech-language pathologists, psychologists, educators, and social workers to help people develop become independent in all areas of their life.

Whether in a private clinic, a hospital centre, or a rehabilitation centre, the interventions of the audiologist aim to reduce the situations of handicap produced by hearing loss or disorders of the vestibular system. Unfortunately, once deafness is diagnosed, it is often irreversible, which leads to a significant period of rehabilitation for those affected. Thanks to precise evaluations, personalized recommendations, and tailored interventions, the audiologist helps patients find solutions that correspond to their needs and lifestyle habits. The audiologist plays a vital role as a healthcare professional, providing expertise, advice, and support throughout the patient’s care journey. Thanks to the contribution of audiologists, many people can regain a better quality of life and overcome challenges related to deafness.