Do you know someone, an adult or elderly person, who is experiencing hearing difficulties and who struggles to understand speech? If so, it’s possible that this person is suffering from presbycusis. This very common issue is often misunderstood or even ignored by those affected. In this article, we will explore presbycusis, its impact on hearing and on the lives of those who suffer from it, as well as approaches to prevention and treatment.

- Definition
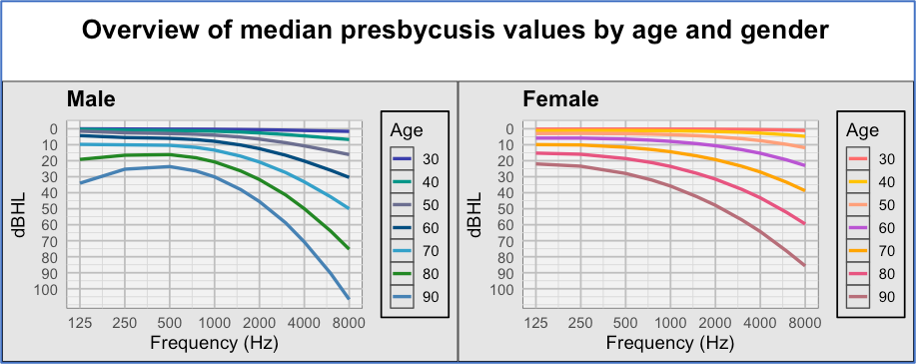
Presbycusis is a progressive hearing loss that occurs naturally with age. Its slow progression can make it difficult for a person to realize they are affected. It initially impacts the perception of high-pitched sounds such as bird songs or consonants like “f” or “s.” As individuals with presbycusis age, this hearing loss tends to extend to lower-pitched sounds, leading to increasing difficulties in understanding speech. Presbycusis is a bilateral and relatively symmetrical hearing loss, meaning that it affects both ears in a similar way. It affects men more than women, possibly due to greater exposure to environmental noise. Its prevalence in the population is 11% among those aged 44 to 54, 25% among those aged 55 to 64, and 43% among those aged 65 to 84. The World Health Organization estimates that by 2025, around 500 million people worldwide will experience difficulties related to presbycusis.
- What are the symptoms of presbycusis?

The first signs of presbycusis can be observed in various situations, such as when a person frequently asks others to repeat themselves, turns up the TV volume to the point of disturbing those nearby, or has difficulty understanding children due to their higher-pitched voices. Other manifestations may include significant difficulties understanding speech in noisy environments, in reverberant places where echoes tend to blur speech, or in the presence of multiple speakers. Those affected might not necessarily complain about not hearing but rather about not understanding speech. The difficulties experienced by individuals are generally proportional to the degree of their hearing loss. In other words, the more severe the age-related hearing loss, the more challenging it becomes for those affected to listen. Besides difficulties in understanding speech, presbycusis can also lead to challenges in localizing surrounding sounds, which can compromise their safety.
Some people might also suffer from tinnitus, as this condition is associated with damage to the hair cells in the cochlea. Presbycusis may also be linked to increased sensitivity to loud sounds, a phenomenon commonly known as “hyperacusis.” However, the precise term for increased sensitivity occurring because of hearing loss is “recruitment.” This happens when the cochlear cells responsible for processing certain sounds are no longer able to do so. The work is then passed on to neighboring cells, leading to increased auditory sensitivity.
It is also common for people affected to reduce their social activities out of fear of being exposed to situations where they might not be able to understand well. Some people tend to deny their difficulties by blaming their conversation partners, claiming that others mumble or do not articulate well. According to the World Health Organization, presbycusis is correlated with a decrease in quality of life and with depression. Research on the negative effects of presbycusis on quality of life indicates that these effects can be categorized into three areas: negative emotional reactions, negative behavioral reactions, and negative cognitive reactions. Negative emotional reactions include feelings of loneliness, isolation, dependence, frustration, depression, anxiety, anger, embarrassment, and guilt. Negative behavioral reactions include pretending (acting as if they hear well when they do not), withdrawal, self-blame, and high demands on oneself and others. Negative cognitive reactions involve confusion, difficulties in concentration, distracting thoughts, reduced self-esteem, and communication disorders.
- Besides age, are there other risk factors?

Aging alone might not fully explain the onset of presbycusis. Indeed, a study conducted by Goycoolea (an otolaryngologist [ENT] and researcher based in Santiago, Chile) and his colleagues in 1986 revealed that age-related hearing loss among the inhabitants of Easter Island, a highly isolated environment, was significantly less pronounced than that observed in people living in noisy urban environments. Samuel Rosen (Emeritus Professor of Otolaryngology at Mt. Sinai School of Medicine in New York, who passed away in 1981) and his collaborators in 1964 observed similar results among residents of a remote region in Sudan. Several factors are known to contribute to the decline in hearing abilities, including noise exposure, ear trauma and diseases, smoking, hypertension, genetic factors, exposure to ototoxic substances (toxic to the auditory system) such as chemical solvents (toluene, xylene, ethylbenzene, benzene, styrene), and the use of certain medications (aminoglycoside antibiotics, cisplatin, loop diuretics, anti-inflammatory agents). It is difficult to distinguish the specific impact of each of these factors on a person’s hearing. Therefore, it is important to consider presbycusis as the result of a combination of all these elements. Adopting a comprehensive preventive approach by avoiding noise exposure and consulting a doctor or pharmacist before starting pharmaceutical treatment is a wise strategy for preventing hearing disorders.
- How is presbycusis diagnosed?

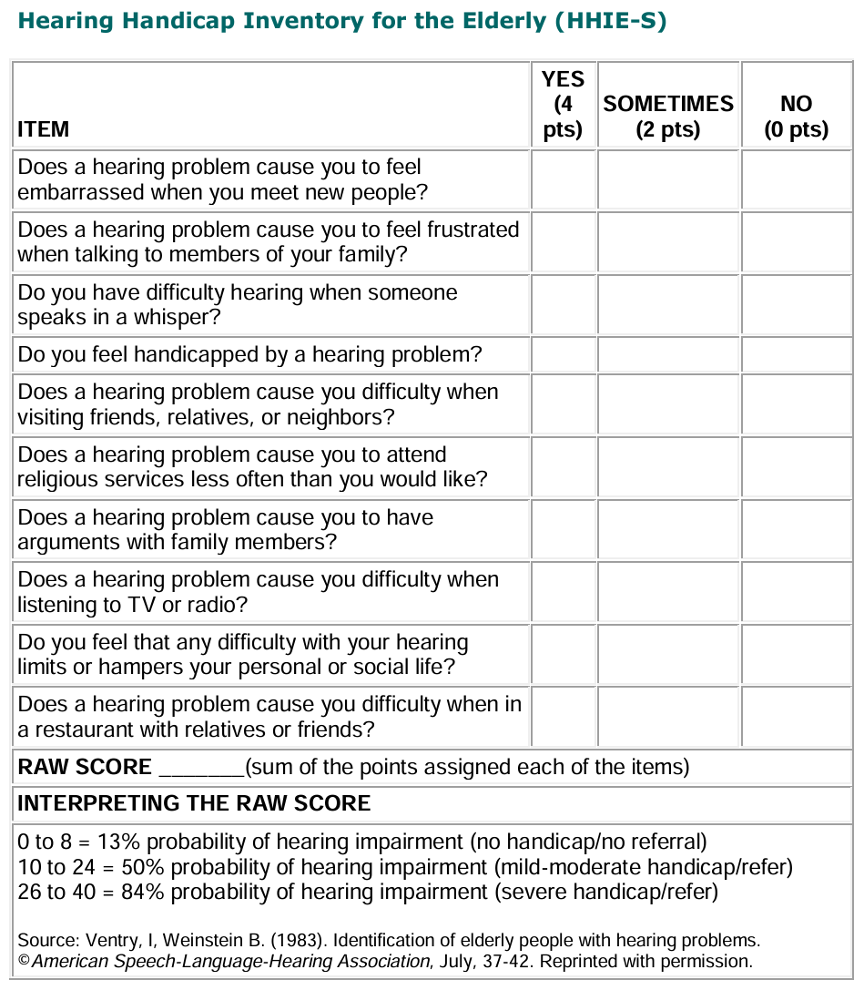
The best way to determine if someone is suffering from hearing loss is to undergo an audiological evaluation by an audiologist. The main tests for diagnosing hearing loss are pure-tone audiometry and speech recognition ability assessment. Pure-tone audiometry determines the minimum sound level at which a person can hear low, mid, and high frequencies. The frequencies typically tested are 250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hertz, which correspond to the range of sounds essential for speech perception. Speech recognition ability assessment can be performed in several ways, such as repeating words or sentences presented at different volumes, in silence or in the presence of competing noise. Additional tests, such as the evaluation of otoacoustic emissions to validate the response of the cochlear hair cells and brainstem evoked potentials to assess the auditory nerve response, can also be conducted. It is generally recommended to undergo annual hearing screening starting at age 60. If this screening is positive, an audiological evaluation by an audiologist is indicated. The following questionnaire can be a good starting point to help someone determine whether an audiological evaluation should be considered.
- How can presbycusis be treated?

The use of hearing aids is the most common method for treating presbycusis. Hearing aids are designed to restore the audibility of speech sounds and to improve the perception of environmental sounds. However, their use comes with some drawbacks. The sound they produce is not identical to the sound that is normally perceived with healthy ears. Getting used to their sound quality and the sensation of having earpieces in the ears may require an adjustment period ranging from a few weeks to a few months. The cost of hearing aids can also be prohibitive. Finally, aesthetics can be an important factor for some users. The most discreet models may not be powerful enough to compensate for more significant cases of presbycusis. The Régie de l’assurance maladie du Québec (RAMQ) may cover the purchase of a single hearing aid for retired individuals. Since presbycusis is a bilateral hearing loss, it requires bilateral fitting for adequate compensation. However, the second hearing aid must be purchased separately by the individual who meets RAMQ criteria and wishes to obtain bilateral fitting.

Assistive Hearing Devices
Assistive hearing devices represent a range of equipment available through RAMQ, under certain conditions, and available over the counter. These include sound transmission systems for television listening. These devices allow a person with hearing loss to listen to the television at a volume suited to their needs without disturbing those around them. Personal amplifiers are also available; they function somewhat like portable microphones: the individual can take them anywhere and point them towards their conversation partners to benefit from sound amplification directly into their ears. There are also telephone amplifiers that provide extra volume for landline or mobile phones. Additionally, there are environmental control devices specifically designed to amplify domestic alert sounds, such as doorbells or smoke detectors. Finally, a wide variety of assistive hearing devices are available to meet the various needs of individuals with presbycusis or any other type of hearing loss. The best way to determine which type of device would suit a person is to consult an audiologist.
Communication Strategies
Communication strategies, which are accessible to everyone, have the great advantage of being free. To prevent communication barriers, a person with presbycusis might choose to minimize noise sources or move away from them before starting a conversation. A good positioning in front of the conversation partner, avoiding backlighting, not only optimizes auditory reception but also facilitates lip-reading. If they feel comfortable, the person can make their conversation partners aware of their hearing challenges, inviting them to slow down their speech, articulate more clearly, or rephrase their messages in simpler terms if necessary. Ultimately, these communication strategies are just as relevant for the person with hearing loss as for their surroundings. Additionally, adapting the environment is among the best approaches to follow, such as reducing noise sources or choosing quieter meeting places.

Cochlear Implant
In cases of advanced presbycusis, a cochlear implant is a relevant alternative. However, the individual’s hearing loss must be classified as severe to profound. Moreover, it is crucial that the person has not experienced prolonged auditory deprivation. A lack of hearing over several years indeed leads to changes in the brain, thereby reducing the likelihood of post-implantation success. Generally, the cochlear implant option is considered when traditional hearing aids can no longer effectively support the person in their daily life. Implantation is a serious commitment. After the operation, the patient must undergo an intensive auditory rehabilitation program for several months to restore their hearing abilities. This procedure is rigorous; it requires a thorough evaluation of candidates and the collaboration of a multidisciplinary team of healthcare professionals. It should be noted that the sound produced by the implant can be unusual and demands a significant adaptation phase. The prospects for success are often better for younger patients. Older candidates, while they may benefit from this technology, must present a favorable prognosis. The key factors are the determination to improve one’s quality of life and the willingness to fully commit to the intensive rehabilitation process.
- Where are we in terms of scientific advancements?
For decades, research efforts have been focused on stimulating the regeneration of damaged cells in the inner ear. However, these techniques are still not applicable to humans. Research is also investigating the development of molecules that could protect the inner ear from the harmful effects of ototoxic substances. Advances in cochlear implant technology are gradually expanding the selection criteria for individuals with significant hearing loss. The continuous development of hearing aid technologies also improves the performance of these devices in listening environments known to be difficult for hearing aids to compensate, such as listening in the presence of competing noise. Government agencies are now more concerned about the hearing loss issues reported in scientific literature. Efforts are being made to increase requirements for auditory safety for workers and the general population, particularly by regulating maximum noise exposure levels.
- Conclusion
Presbycusis is an unavoidable reality in our aging society. Its manifestations, ranging from simple difficulty discerning high-pitched sounds to more profound deafness, disrupt not only the daily lives of those affected but also influence their social interactions, emotional wellbeing, and cognitive abilities. It is essential to recognize that behind every person experiencing hearing problems lie unique challenges and complex emotions. The solutions offered, though varied and constantly evolving, require an individualized approach. From hearing aids to cochlear implants, and assistive hearing devices, each intervention must be carefully tailored to the specific needs of individuals. Moreover, beyond medical and technological treatments, the importance of the involvement of loved ones and communication strategies cannot be overlooked. A global awareness of this issue, combined with a collective commitment to research, innovation, and support, is essential for improving the quality of life for those affected by presbycusis.
Suggested readings
- The peripheral auditory system
- The central subcortical auditory system
- The auditory cortex
- Speech perception: a complex ability
- The profession of speech-language pathologist
- Audiology and the work of audiologists
- The McGurk effect
- Speech Perception in Noise: Facilitatory Mechanisms of the Peripheral Auditory System
- Can musical practice improve listening to conversations in noise?