After several months of analysis and writing, the results of our survey on occupational voice users are now published!
Little known to the public, invisible to the naked eye, voice disorders can nevertheless have serious consequences for occupational voice users such as teachers: more frequent absenteeism due to illness, stress, burnout, professional reorientation, increased workload for colleagues, decreased workplace productivity (Brito Mota et al., 2019; Kyriakou et al., 2017; Giannini et al., 2015; Martins et al., 2014), etc.
Studies carried out in other countries, mainly in Europe, the United States and Australia, have shown that less than half of those with a voice disorder consult a health professional (Da Costa et al., 2012) and that most workers typically do not receive adequate training about voice disorders (E.g., Van Houtte et al., 2010). In addition, in the scientific literature, a lack of clarity remains regarding the risk factors associated with voice disorders, which hinders the development of prevention programs based on scientific data.
What is the situation in Quebec? Our study aimed to provide a portrait of the vocal health of Quebec occupational voice users and to document their knowledge of vocal health. Our study also aimed to identify the risk factors associated with voice symptoms.
To achieve these goals, we designed and shared an online survey via email or Facebook with many organizations, including teachers’ unions, school principals, daycares, fitness centers, etc. We collected over 800 responses! The main characteristics of our respondents are illustrated in Figure 1.
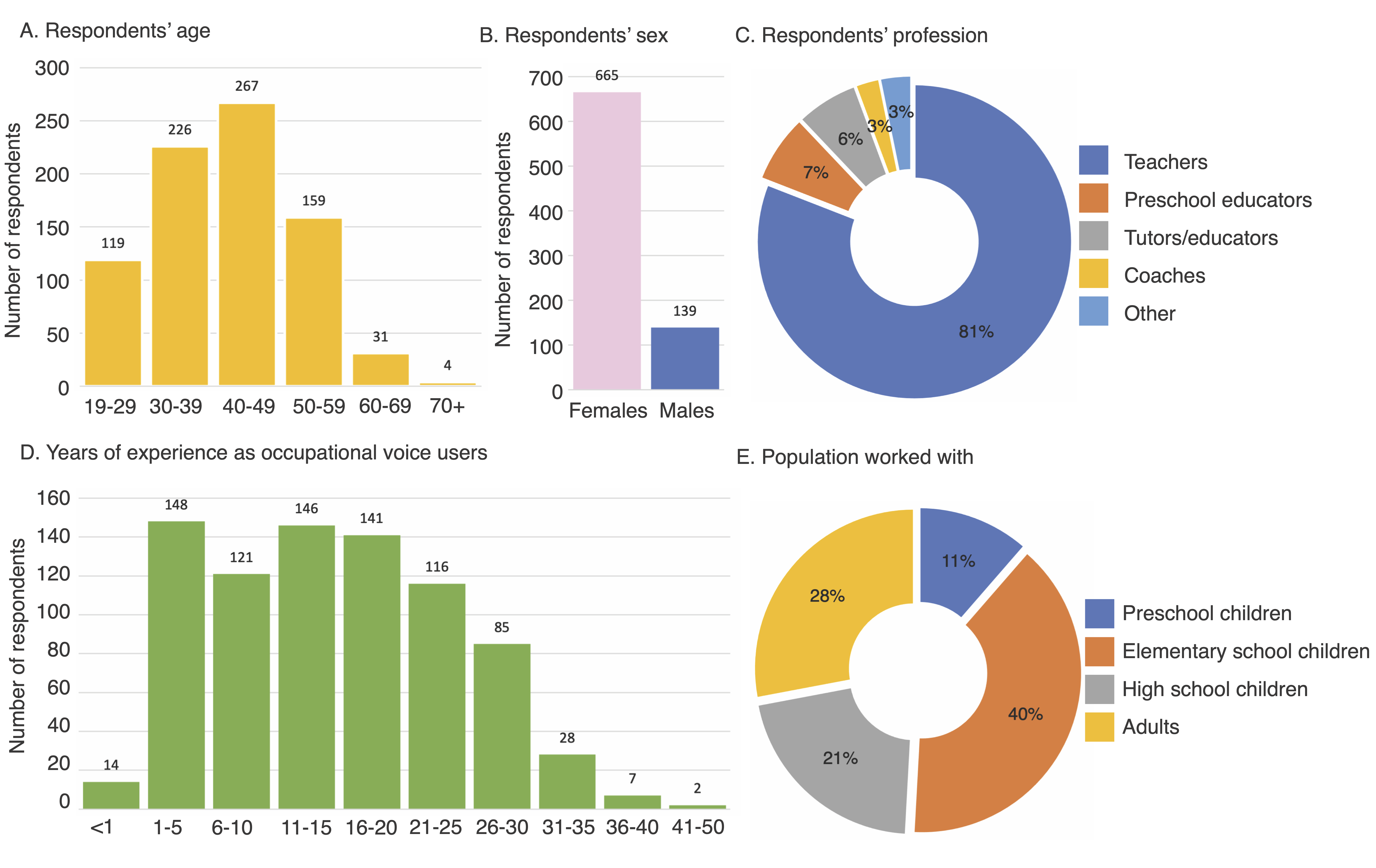
Figure 1. Illustration of the main characteristics of respondents.
The results indicate that about 10% of respondents had already been diagnosed with a voice disorder. However, nearly 70% of them often or very often had at least one symptom of voice disorder (see Figure 2A and 2B). 24.5% of respondents reported having consulted a healthcare professional (doctor, otolaryngologist [ENT] or speech therapist) for voice-related problems. These results suggest that people who use their voice as a work tool are at risk of developing a voice disorder, but that they do not often consult professionals, despite the fact a significant number of respondents considered themselves at risk of developing a voice disorder (see Figure 2C) or were worried about it (see Figure 2D).
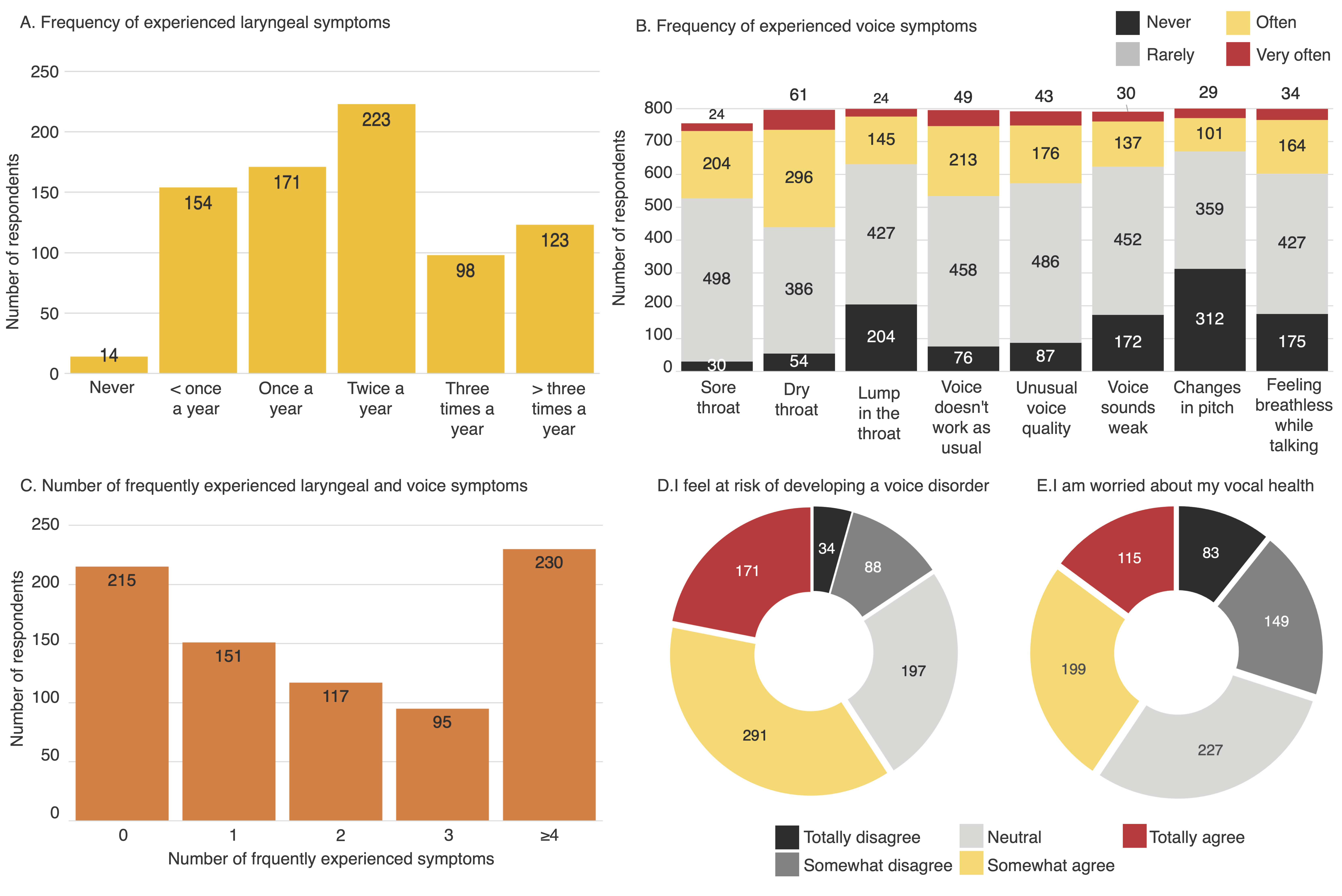
Figure 2. Illustration of the number of respondents experiencing symptoms affecting the larynx and voice or having concerns about their voice health.
Our analyses also identified factors associated with voice symptoms. The number of symptoms often or very often experienced, as well as the frequency of symptoms, were higher among women, and in those with a respiratory disorder, acid reflux or a hearing problem. Having seasonal or dust allergies was also associated with a greater risk of experiencing voice symptoms. Working in a noisy environment (with continuous background noise or people talking in the background) or working with preschool children increased the risk of experiencing voice symptoms. In contrast, more years of work experience was associated with a slightly lower risk of experiencing voice symptoms.
Our results contribute to current understanding of the risk factors for voice disorders. This knowledge is important for the development of prevention and awareness programs for voice disorders. For example, a preventive measure for the workplace could be to reduce the sources of ambient noise, which can lead to a decrease in workers’ vocal intensity and ultimately reduce the risk of developing voice disorders.
Regarding knowledge about voice health, our survey revealed that a majority of respondents had never received information about voice disorders during their academic training (94.6%) or from their employer (97.6%). Moreover, only 36.4% knew at least one method to protect their voice and less than half (47.7%) knew which health professionals can treat voice disorders. These findings highlight a huge need for education about vocal health among occupational voice users. Training targeting employers could also be beneficial. Indeed, less than 10% of respondents mentioned that their employer implemented preventive measures against the development of voice disorders (use of a voice amplifier, soundproofed room, reduced number of people per group). Additionally, although 71.4% of survey respondents agreed that a voice problem was a valid reason for taking a sick leave, only 25% believed their employer would agree with this statement. Thus, employers may not be aware of the consequences of voice disorders and how to prevent them.
What is the next step? Empirical studies are needed to document more objectively the prevalence of voice disorders in occupational voice users to verify and extend our results to other kinds of occupational voice users such as radio hosts, voice actors and comedians.
Finally, our study highlights a need for training in vocal health, a situation that has long been denounced by vocal health specialists. We hope that our results will help educate decision-makers and academic institutions.
To access the full text of the scientific article: Brisson, V., Fournier, C., Pelletier, A., Joyal, M., Defoy, L., & Tremblay, P. (2022). Vocal Health and Vocal Health Knowledge Among Occupational Voice Users in the Province of Quebec. Journal of Voice.
References:
Da Costa, V., Prada, E., Roberts, A., & Cohen, S.M. (2012). Voice disorders in primary school teachers and barriers to care. Journal of Voice, 26:69–76.
de Brito Mota, A.F., Giannini, S.P.P., de Oliveira, I.B., Paparelli, R., Dornelas, R., & Ferreira, L.P. (2019). Voice disorder and burnout syndrome in teachers. Journal of Voice, 33:581. e516–581. e587.
Giannini, S.P.P., Latorre, M.dR.D.dO., Fischer, F.M., Ghirardi, A.C.dA.M., & Ferreira, L.P. (2015). Teachers’ voice disorders and loss of work ability: a case-control study. Journal of Voice, 29:209–217.
Kyriakou, K., Petinou, K., & Phinikettos, I. (2017). Risk factors for voice disorders in university professors in Cyprus. Journal of Voice, 32:643. e641–643.e649.
Ma, Z., Bullen, C., Chu, J.T.W., Wang, R., Wang, Y., & Singh, S. (2021). Towards the objective speech assessment of smoking status based on voice features: a review of the literature. Journal of Voice.
Martins, R.H.G., Pereira, E.R.B.N., Hidalgo, C.B., & Tavares, E.L.M. (2014). Voice disorders in teachers. A review. Journal of Voice, 28:716–724.
Van Houtte, E., Claeys, S., Wuyts, F., & Van Lierde, K. (2011). The impact of voice disorders among teachers: vocal complaints, treatment-seeking behavior, knowledge of vocal care, and voice-related absenteeism. Journal of Voice, 25:570–575.
Further readings: